


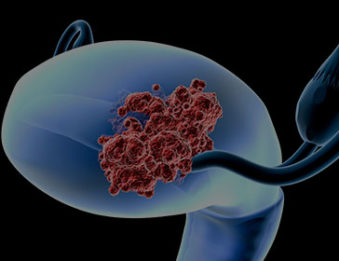
Five main types of cancer affect a woman’s reproductive organs: cervical, ovarian, uterine, vaginal, and vulvar. As a group, they are referred to as gynecologic cancers. Each gynecologic cancer is unique, with different signs, symptoms, and risk factors.
All women are at risk for gynecologic cancers, and risk increases with age. When gynecologic cancers are detected early, cure rates are excellent.
There are five main types of cancer affect a woman’s reproductive organs:
Although these cancers are all included in this subset, each type has its own unique qualities. We encourage you to contact our center to learn more about the various stages.
If you have abnormal vaginal bleeding, talk to your radiation oncologist right away. You should also see a radiation oncologist if you have any other warning signs that last for two weeks or longer and are not normal for you. Symptoms are most often caused by something other than cancer, but the only way to know is to see a radiation oncologist.
Signs and symptoms are not the same for everyone and each gynecologic cancer (cervical, ovarian, uterine, vaginal, and vulvar cancers) has its own signs and symptoms.
Gynecologic cancers are treated in several ways. It depends on the kind of cancer and how far it has spread. Treatments include surgery, chemotherapy, non-chemotherapeutic systemic therapy, and radiation therapy. Women with gynecologic cancer often receive a combination of treatment.
Our oncologists are also experienced in other various forms of cancer, including:
An obstetrician/gynecologist who specializes in the diagnosis and treatment of women with cancer of the reproductive organs.
Any woman who has been diagnosed with or is suspected to have a gynecologic cancer.
Cervical dysplasia is a precancerous condition of the cervix. Similar terms include carcinoma in situ and squamous intraepithelial lesion, or SIL.
Because precancerous lesions rarely cause symptoms, timely diagnosis of cervical dysplasia depends on regularly having a Pap smear. In general, sexually active young women should have a Pap smear once a year. If a Pap smear is abnormal, the physician will perform further tests.
Since mild dysplasia can spontaneously disappear, in some cases women can safely choose surveillance, as long as the site is frequently examined by a physician; however, treatment options should be discussed.
Testing positive for certain HPV virus types is the largest risk factor for developing cervical cancer. Multiple sexual partners in your lifetime (more than five), intercourse at an early age and smoking are also contributors.
Many times there are no symptoms. A Pap smear that is abnormal is usually the first sign of possible cancer. Some women may have persistent bleeding after intercourse, irregular menstrual spotting or possibly postmenopausal bleeding.
A Pap smear is usually done first. If it is abnormal, another test called a colposcopy is usually done. A biopsy (a procedure in which a small amount of tissue is taken from the cervix) is needed for the pathologist to make a microscopic diagnosis.
If a woman has cervical cancer, surgery, chemotherapy and/or radiation therapy may be recommended. The best treatment for an individual woman will vary, depending on her health history, the stage of the disease and issues related to childbearing.
LEEP is the abbreviation for loop electrosurgical excision procedure. It is one of the most common techniques used for the treatment of cervical dysplasia.
For some women, a deeper, cone-shaped piece of tissue must be removed from the cervix in order to make a correct diagnosis or to treat cervical cancer.
Risk factors include obesity, nulliparity (never having been pregnant), diabetes, Tamoxifen use, taking estrogen replacement without progesterone, anovulation (menstrual cycles without ovulation) and polycystic ovarian syndrome. Women with these factors have been exposed to either excessive levels of estrogen exposure or to unopposed estrogen.
Many women have postmenopausal bleeding. Others may have perimenopausal intermenstrual bleeding episodes or have significant changes to their menstrual cycle, usually excessive bleeding. Women with any of these risk factors should be especially alert to any abnormal bleeding.
A thin straw is inserted into the uterus to obtain a small amount of tissue for diagnosis. This is called an endometrial biopsy, and is most often done in a radiation oncologist’s office. Sometimes more tissue is needed for diagnosis, and a dilatation and curettage is performed under anesthesia.
Most often, surgery is recommended to remove the uterus, the ovaries and the fallopian tubes. Sometimes, lymph nodes are removed at the time of the surgery. In addition, radiation therapy, chemotherapy and possibly hormone treatment may be utilized.
All women are at risk for ovarian cancer. Women with first degree relatives with ovarian cancer, a family history of breast cancer, and women with Lynch II syndrome are at a higher risk for developing the disease, especially after menopause.
Recent studies show that many women who are diagnosed with ovarian cancer complain of such symptoms as bloating, increased abdominal size and urinary symptoms. Because these are such vague symptoms, diagnosis can be difficult. Women with a new onset of these symptoms need a pelvic exam and possibly an imaging study if the condition does not improve after a few weeks with conservative treatment.
As there is no screening test for ovarian cancer, unlike the Pap smear for cervical cancer, diagnosis of ovarian cancer requires surgery and the removal of the suspicious mass. The extent of the surgery — including whether fertility can be preserved — is best decided in conference with a gynecologic oncologist.
Surgery is always required, often followed by chemotherapy. Research into the best way to administer chemotherapy is rapidly evolving, so devising the best course of treatment is done in consultation with a gynecologic oncologist.
The most likely association is a history of HPV (human papilloma virus), usually in the form of genital warts. There is also probably an association with multiple sex partners and smoking, especially in women under 65 years old. Elderly women may develop vulvar cancer after years of chronic vulvar irritation. Embarrassment about seeking care for these irritations can lead to the development of an otherwise preventable cancer.
Most women develop a mass or a non-healing sore in their genitalia, the most common site being their labia majora. Many times they experience chronic itching and eventual pain. Any abnormal discharge or bleeding from the genital area can also be a sign of vulvar cancer.
A biopsy (tissue sample) should be taken from the area of concern and sent to a pathologist for microscopic examination.
A colposcopy should be performed of the external and internal genitalia, to identify all areas involved in either precancerous changes or invasive cancer. Smaller cancers are then surgically removed, along with the lymph nodes in the groin. Larger cancers require treatment with radiation therapy and chemotherapy.
The most likely association is a history of HPV (human papilloma virus), usually in the form of genital warts. There is also probably an association with multiple sex partners and smoking, especially in women under 65 years old. The most important risk factor is a previous diagnosis with cervical dysplasia or cancer. Radiation oncologists caring for women with a history of cervical dysplasia or cancer need to obtain regular Pap smears from the vaginal canal.
These are precancerous conditions of the vulva or vagina. Similar terms include carcinoma in situ and vaginal or vulvar intraepithelial neoplasm, often abbreviated as VAIN or VIN.
Most vaginal dysplasias are detected by Pap smears, followed by a colposcopy and selected biopsies the removal of small pieces of tissue which are examined microscopically. The diagnosis of vulvar dysplasia depends primarily on biopsies, after a woman has reported nonhealing sores, wart-like growths, persistent itching or other problems to her physician.
Mat-Su Valley Cancer Center is a specialty healthcare facility dedicated entirely to the treatment of many kinds of cancer. Contact us at 907-707-1333.